About TUG Flap Breast Reconstruction
TUG Flap Donor Site: Thigh
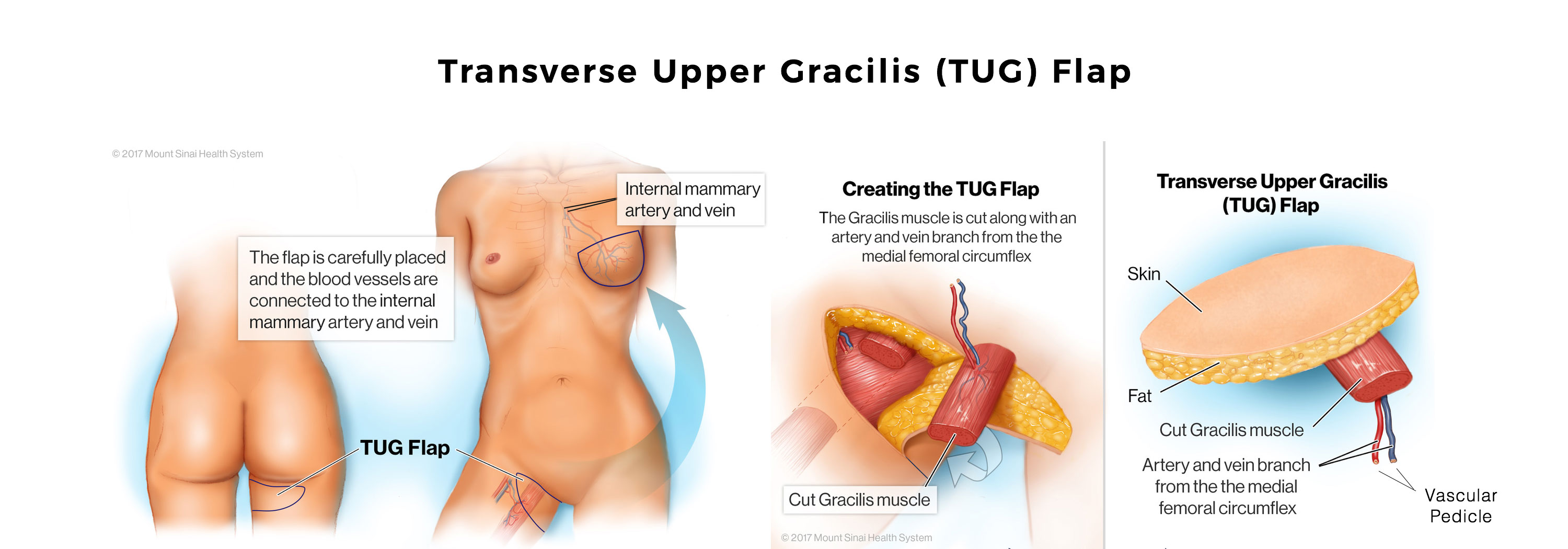
The TUG or transverse upper grades gracillis flap is taken from the inner thigh. This flap is used for breast reconstruction in patients who cannot, or would rather not use their abdomen as a donor site.
This flap uses a small muscle called the Gracillis , and takes its blood supply from that muscle. The skin and fat that is used with this flap is very similar to the territory of the PAP flap. Since the PAP procedure does not sacrifice any muscle and can be placed further back, just underneath the buttock crease, the PAP flap has largely replaced the TUG.
Common Questions about the TUG Flap
Breast Reconstruction Procedure
A woman may be considered a candidate for TUG (Transverse Upper Gracilis) flap breast reconstruction if she meets certain criteria. The TUG flap technique utilizes tissue from the inner thigh, specifically the gracilis muscle and surrounding skin and fat. Therefore, a woman needs to have sufficient tissue in the inner thigh to create a breast mound of the desired size.
UG (Transverse Upper Gracilis) flap breast reconstruction offers several benefits for women considering autologous breast reconstruction. Here are some potential advantages of TUG flap reconstruction:
- Use of natural tissue: TUG flap reconstruction utilizes the patient’s own tissue from the inner thigh, including the gracilis muscle, skin, and fat. This results in a breast reconstruction that feels and behaves more like a natural breast compared to implant-based reconstruction.
- Avoidance of implants: Some women prefer to avoid the use of breast implants for reconstruction. TUG flap reconstruction allows for breast reconstruction without the need for implants, using the patient’s own tissue instead.
- Consistency in body contour: The tissue from the inner thigh used in TUG flap reconstruction closely matches the texture and consistency of breast tissue, resulting in a reconstructed breast that closely resembles the natural breast in terms of appearance and feel.
- Preservation of muscle function: The TUG flap technique preserves the function of the gracilis muscle, which is primarily responsible for hip adduction (bringing the thigh toward the midline). Preserving the muscle function can help maintain overall lower extremity strength and function.
- Scar placement: The incisions for TUG flap reconstruction are typically placed in the inner thigh region, which allows for scar concealment in areas that are often covered by underwear or swimsuits.
- Potential for simultaneous thigh contouring: In some cases, excess skin and fat in the inner thigh area can be removed during the TUG flap reconstruction procedure, providing the added benefit of thigh contouring.
Yes, TUG (Transverse Upper Gracilis) flap breast reconstruction can be used as part of a combination flap breast reconstruction approach. Combination flap reconstruction involves utilizing multiple donor sites to harvest tissue for breast reconstruction, combining different autologous flap techniques to optimize the aesthetic outcome and address specific patient needs.
In combination flap breast reconstruction, the surgeon may combine the TUG flap with other flap techniques such as the DIEP (Deep Inferior Epigastric Perforator) flap, SGAP (Superior Gluteal Artery Perforator) flap, or other suitable options depending on the patient’s anatomy and individual requirements. The specific combination of flaps chosen will depend on factors such as the amount of available donor tissue, the desired breast size and shape, and the overall surgical plan.
Combining different flaps allows the surgeon to tailor the reconstruction to meet the patient’s individual needs and optimize the aesthetic outcome. It can provide additional tissue volume, enhance the overall contour and shape of the breast, and address specific challenges or limitations posed by using a single flap technique alone.
Gradually, blood vessels and nerves grow into the transferred tissue. Scars fade, and the end result is a breast reconstruction that looks and feels and behaves exactly like a normal breast. The only difference is that there is no breast tissue inside it, and therefore no risk of breast cancer in the transferred tissue.
Natural tissue breast reconstruction has several benefits compared to other methods of breast reconstruction. Here are a few key benefits:
- It uses a woman’s own natural tissue, which means that it is less likely to be rejected by the body.
- It doesn’t require the use of implants, which can cause complications such as scarring, infection, and hardening of the breast tissue.
- It doesn’t sacrifice any muscle, which means that women can retain their natural shape and function.
- It can be performed at the same time as a mastectomy, which can save time and reduce the overall number of surgeries that a woman needs to undergo.
- It can help women feel more comfortable and confident in their own bodies, which can improve their quality of life.
Overall, natural tissue breast reconstruction can provide women with a more natural and safe option for restoring their breasts after a mastectomy.
“Dr. Levine is an outstanding Doctor. He is a wonderful human being and a highly skilled surgeon. My results are nothing short of miraculous. There is no one like Doctor Levine. He is an artist and a true professional.”

Dr. Joshua L. Levine, MD, FACS
World Leading Authority in Perforator Flap Breast Reconstruction
Based in New York, New Jersey, and Connecticut
Meet Dr. Joshua L. Levine,
World-Renowned in the Art and Science of Natural Tissue Breast Reconstruction
Dr. Joshua Levine is a world-renowned perforator flap breast reconstruction surgeon. Meaning, all of his breast reconstruction procedures, are muscle-sparing, using only your own natural tissue to restore your breast(s).
With his advanced techniques, such as stacked combination flaps, or utilizing the delay phenomenon in staged-immediate reconstruction, all women, no matter how thin and no matter what body type, are candidates for natural tissue, muscle-sparing, implant-free breast reconstruction.
As Seen On: US News & World Report, diepflap.com