Breast Reconstruction: Your Right, Your Choice
Transcription of above presentation:
Hello! My name is Dr. Joshua Levine. I am a reconstructive plastic surgeon in New York City, and I’ll be talking to you today about options for breast reconstruction. This is a talk that has traditionally been given by Kathy Steligo and it kind of goes through the book that she wrote called The Breast Reconstruction Guidebook, and I highly recommend this book. It’s very comprehensive and an excellent explanation of all of breast reconstruction options. She’s unable to give the talk this year and she’s been kind of to lend me her slides, and so this is Kathy’s talk but I’ll be giving it. So, welcome.
We’ll be talking today about what is a mastectomy; what are the options after mastectomy; very briefly touch on no reconstruction, which is called going flat. Then, we’ll talk about the different options related to breast reconstruction, how to choose a plastic surgeon, and how to make some of these difficult decisions.

So, after mastectomy it’s not absolutely required that patients have reconstruction, although it is considered to be the best option by many of us in the field and it is the standard of care. So, no reconstruction typically is accompanied by prosthesis or reconstruction. Reconstruction could be done either with implants or the patient’s own body tissue, which we call autologous reconstruction.
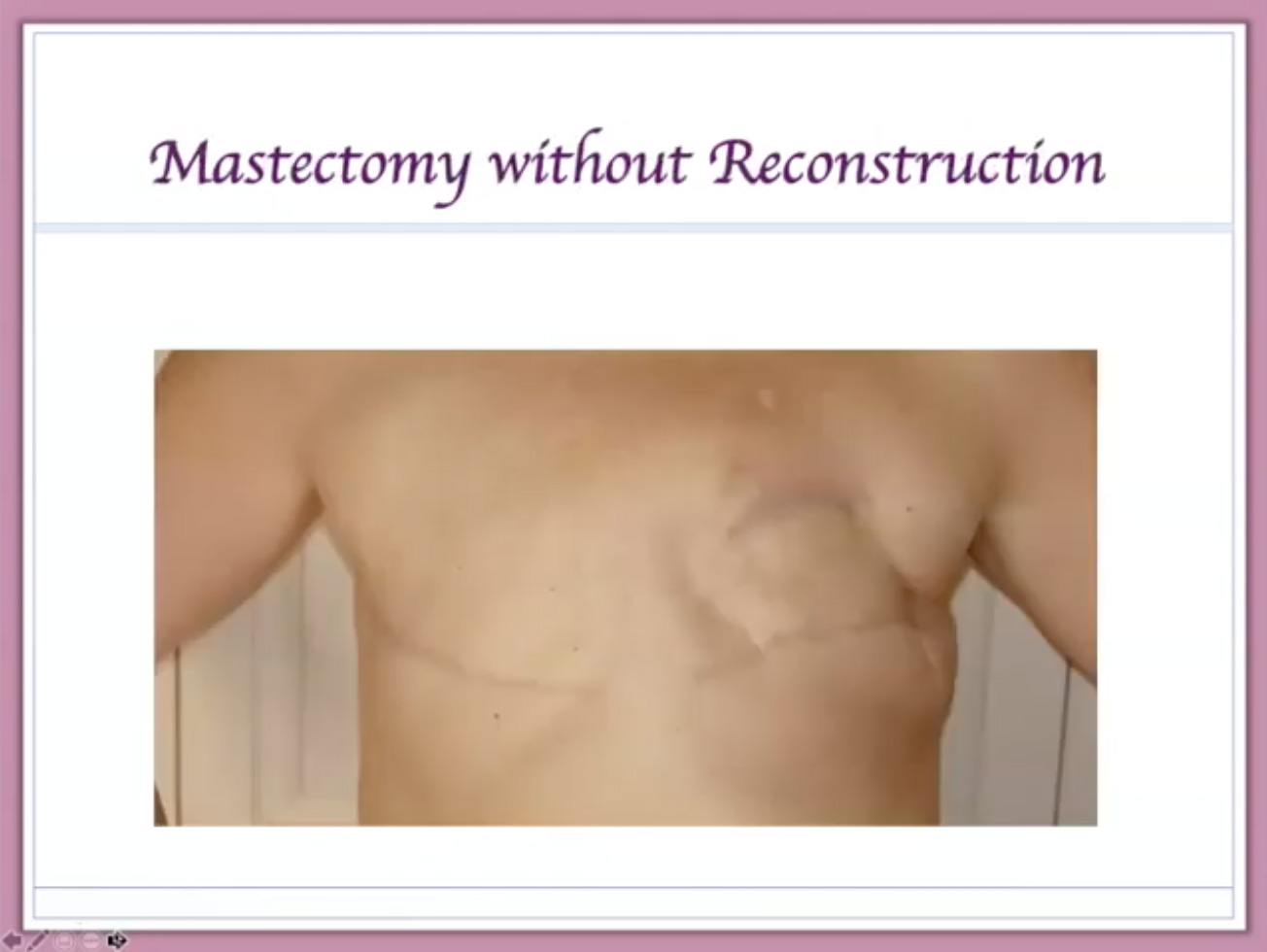
If patients choose to have no reconstruction, the skin of the chest is closed as a straight line after the mastectomy and it looks something like that. Patients can elect then to either wear a prosthetic device in their bra or not, depending upon the patient’s preference.
But reconstruction, again, is the standard of care, and it is covered by medical insurance. There was a law passed in 1998 which ensures that all women who undergo mastectomy are covered for all procedures related to mastectomy. If the insurance policy covers mastectomy, it must cover all other procedures related including all phases of breast reconstruction. While this doesn’t necessarily mean that you’ll get the procedure, physician and facility of your choice, you typically can fight for that and your insurance company should cover it.
The goal of reconstruction is to recreate a natural and normal-looking breast that looks natural with and without clothing. There are lots of different types of reconstruction, and there’s not one right reconstruction that is correct for all patients. So, it’s very, very important for everyone to avail themselves of enough information to make a decision that is perfect for you as an individual. So, before we get into what the options are relative to breast reconstruction, let’s talk a little bit about what is a mastectomy.
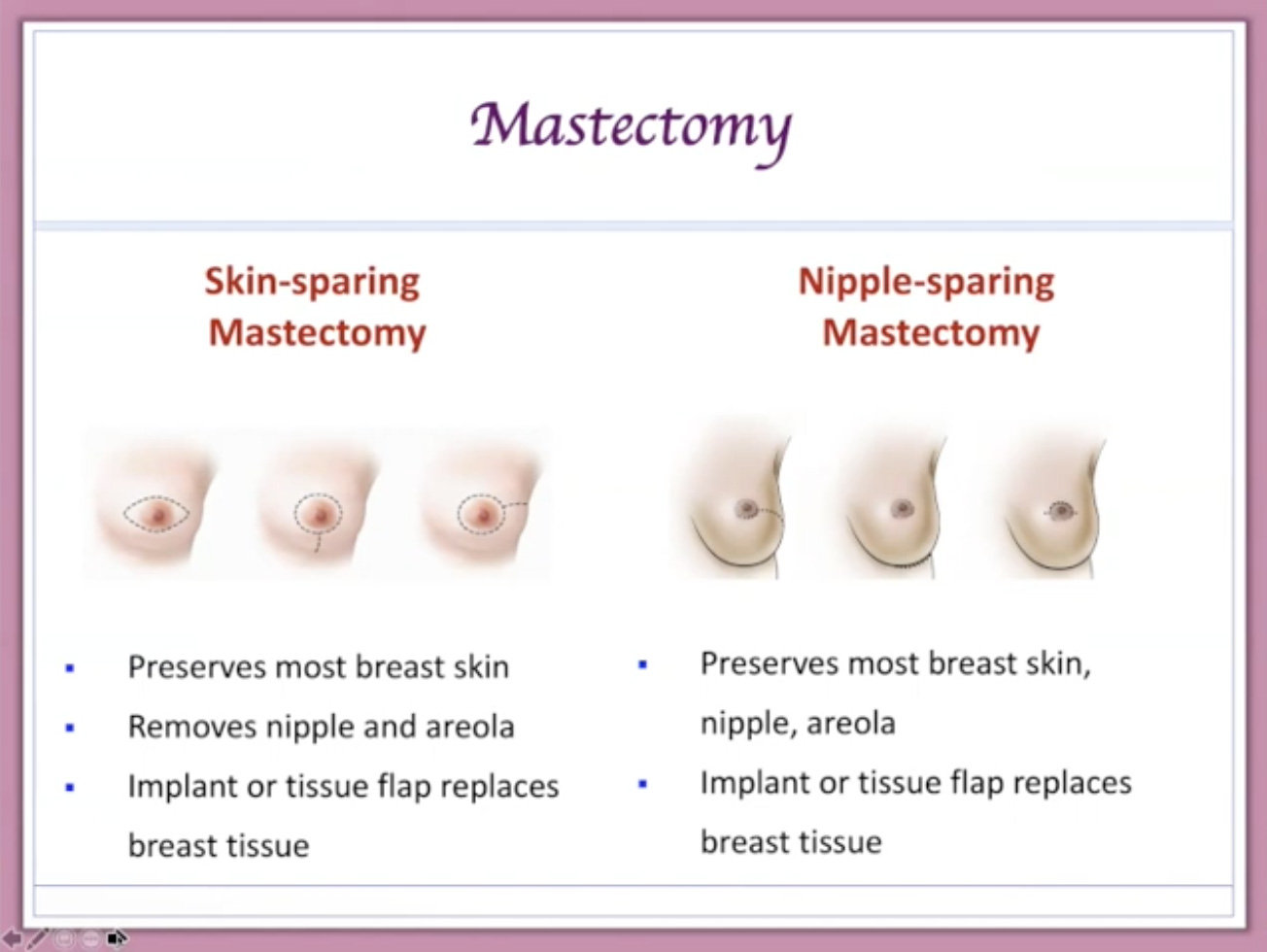
A mastectomy is done typically for cancer but also for patients who are at high risk for cancer, namely those in the BRCA community who are at high risk, and in that case the mastectomy would be called prophylactic meaning that it’s done to prevent cancer. The typical mastectomy is done with the removal of the nipple and the areola. That is called a skin-sparing mastectomy. The reasonable it’s called a skin-sparing mastectomy is because the skin that overlies the breast tissue is preserved. There should be no breast tissue within the skin of the breast. So, that can be safely preserved.
Also, in some cases the nipple/areola can also be preserved and this is called a nipple-sparing mastectomy. Who’s a candidate for nipple-sparing mastectomy? Well, the reason why we would do a nipple-sparing mastectomy is because it does provide a much better cosmetic outcome. From an oncological point of view, a patient is a candidate for nipple preservation if they’re prophylactic. But also, if the skin is not anywhere near the tumor, if the cancer is early stage and it doesn’t involved the nipple, cancer patients may also be candidates for nipple preservation. In order to ensure that there is no cancer in or near the nipple, a biopsy is typically taken at the time of the mastectomy, and if the cancer does involve the nipple the nipple may be removed during or even after the mastectomy. At that point, then the reconstructive surgeon is there to fill in the empty skin envelope.
With nipple preservation, again, you do have a better cosmetic outcome, but there are some issues that may arise. For example, the nipples may flatten, you can expect to have some loss of sensation, and in the worst-case scenario the nipple may not survive the mastectomy. But, you ought to know also from an oncological point of view that the survival and recurrence rate is the same as that of a standard skin-sparing mastectomy.
Now, there may be another reason not to do a nipple preservation and that would be if the patient has very large saggy breasts, which we call ptotic breasts, and you can imagine that, in those scenarios, the nipple is not in an optimal position for a reconstructive breast and, therefore, when the reconstruction is done the nipple is not repositioned appropriately. Now, in order to deal with this situation, the nipple can be repositioned prior to the mastectomy. This is done with a breast reduction and a nipple lift three months prior. And so, this can be done in prophylactic cases.
So, once the mastectomy is done, the plastic surgeon is there then to do the breast reconstruction. Now, there are two main categories of breast reconstruction. One category is implant reconstruction, the other category is autologous reconstruction.

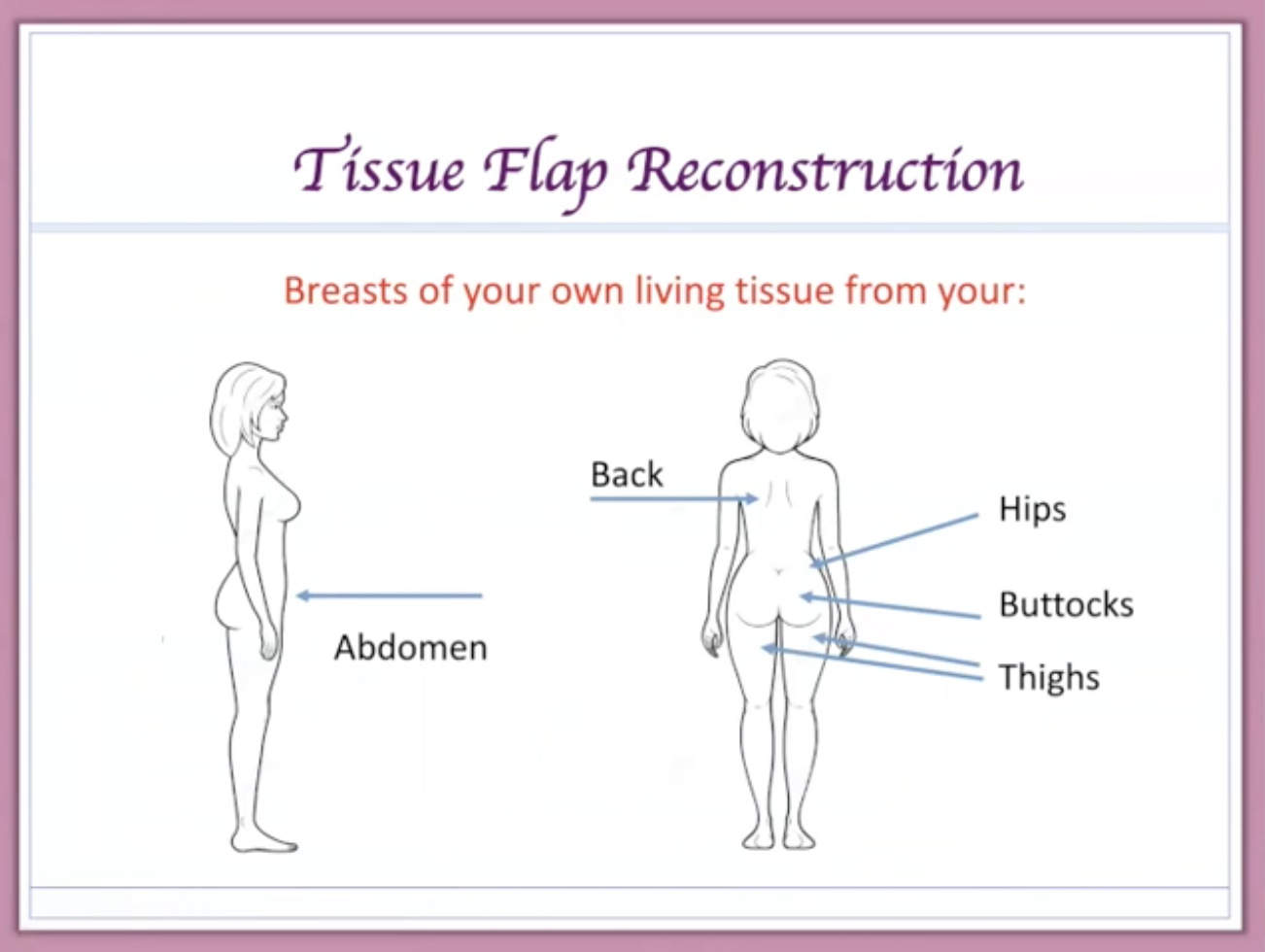
An autologous reconstruction is a term that means that the plastic surgeon uses the patient’s own body tissue to reconstruct or remake the new breast. When we talk about autologous reconstruction, again, we’re talking about using the patient’s own body tissue, and body tissue in this case consists of skin and fat to make a new breast. Now, there are autologous tissue reconstructions which we also call flap reconstructions or flap procedures, which do include muscle, but typically what we want for a breast reconstruction is skin and fat, and in order to supply that for breast reconstruction we call those operations perforator flaps, which I’ll describe in more detail.
On the implant side, we have implants that are made out of silicone. Silicone is the outer shell, but the inside can be filled with either silicone gel or saline. So, there are options there. In the traditional implant reconstruction, the patient undergoes a series of expansions in order to create the pocket that would accommodate the reconstruction or the implant, but even more lately, some surgeons are offering immediate implant reconstruction or direct to implant. Almost all of these procedures related to implants do involve a substance called Alloderm, which I’ll describe momentarily.
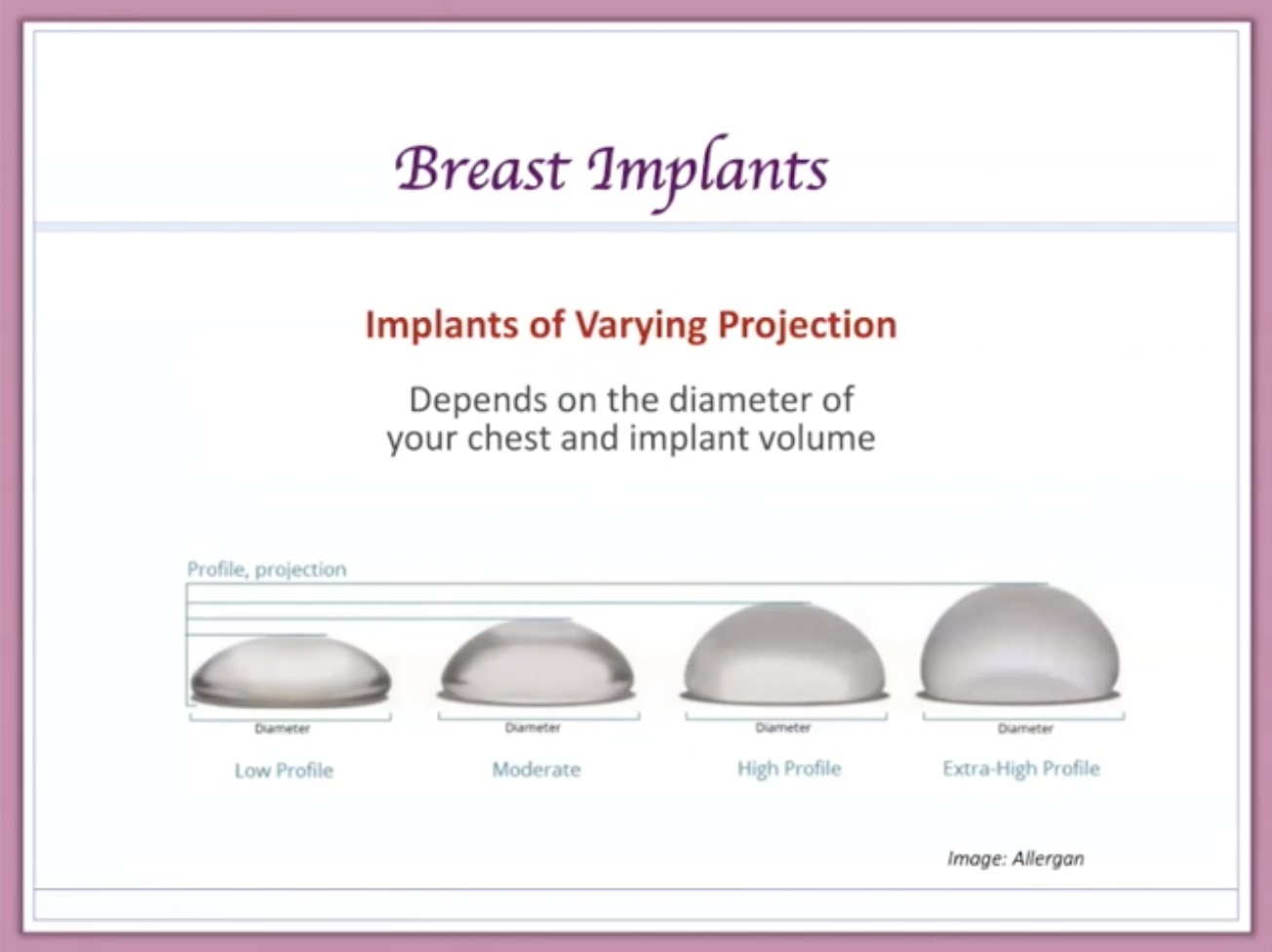
Implant reconstruction, again, can be done with silicone- or saline-filled implants, there are all kinds of different implants to choose from, and the implant that’s appropriate for you will depend upon your situation and also your surgeon’s preference and level of experience. The saline-filled is surrounded, again, by a silicone shell. There are advantages and disadvantages to either saline or silicone, and these are some of the things that you will talk about with your reconstructive surgeon.
The way that these procedures are done, again, typically, is with expansion. What that means is that at the time of the mastectomy the reconstructive surgeon comes in and places not the implant but an expander underneath the muscle in the chest, which is called the pectoralis muscle.
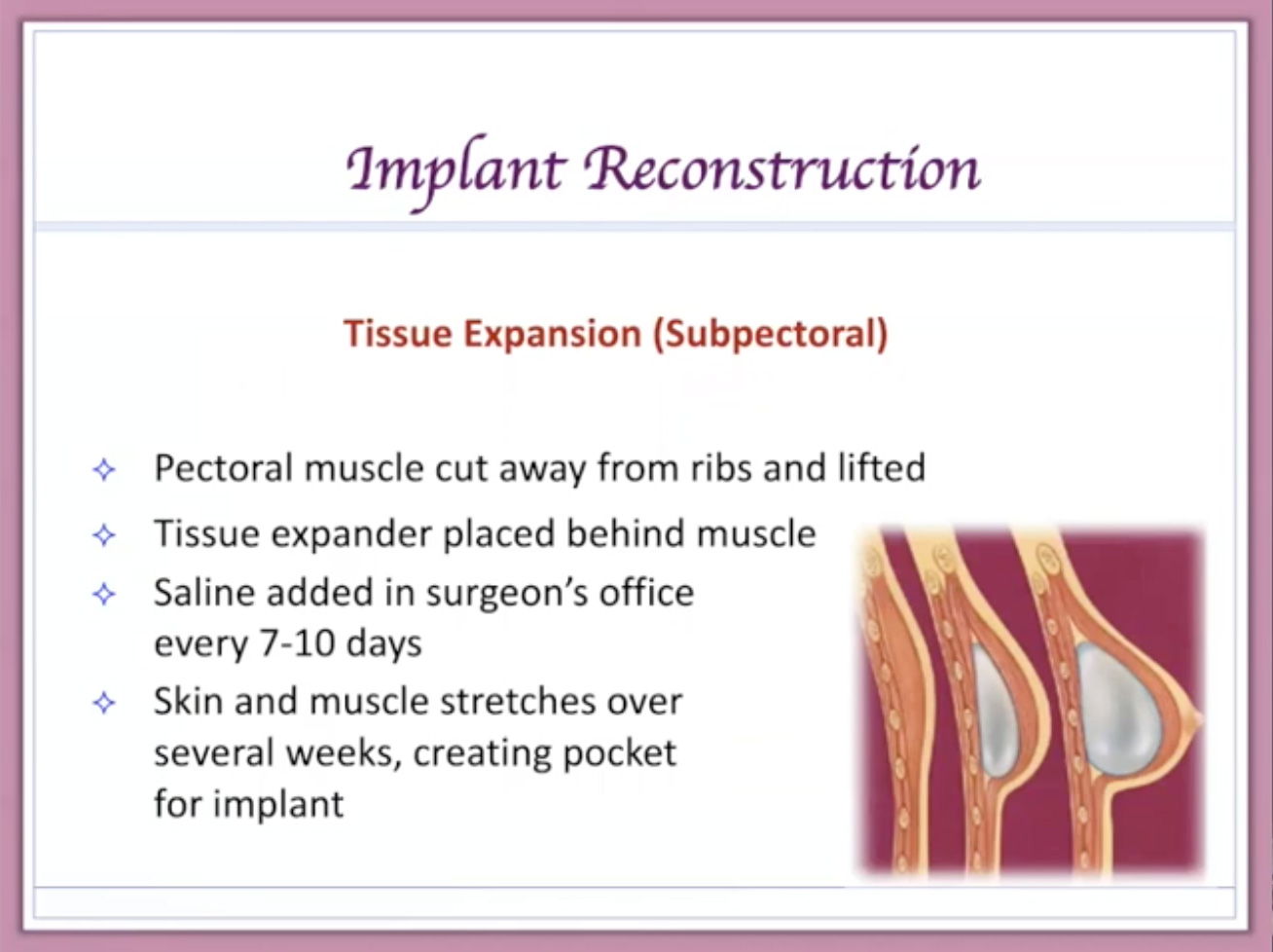
And then also with a piece of Alloderm this is covered over with the muscle and the skin and closed up, deflated such that over the next several months the patient returns to the plastic surgeon’s office and the expander is injected with saline in order to expand to the appropriate size and shape so that once this has been achieved the expander is removed and is exchanged for the final implant. The expansion takes anywhere from one to three months, and then after the expanded pocket is created patient is taken back to the operating room and the expander is replaced with a permanent implant, and at that time the nipple can be reconstructed.
One new development with respect to implant reconstruction is called the prepectoral operating room over the muscle implant, and this has the distinct advantage of not having to lift up the pectoralis muscle so that the implant sits on top of the muscle. This can be much more comfortable ultimately for the patient, but it does require that the entire implant is covered over with a substance called Alloderm because the muscle of the chest is not being used and just skin alone is not enough to cover the implant without using something. So, Alloderm is used and this also called acellular dermal matrix. This is a substance that is harvested from cadavers. It is treated such that no human cells or DNA are inside of it—it’s only the collagen mesh—and it’s used as a barrier or a cushion between the implant and the patient’s skin in cases where the implant is placed on top of the muscle, again, prepectoral, as opposed to underneath the muscle.
The two types of implant reconstruction, again, using the subpectoral underneath does require expansion and usually requires a small piece of Alloderm at the bottom part to cover over where the muscle doesn’t reach, and then the prepectoral or over the muscle, where the muscle is not used, this implant is put in in one step and the entire implant is covered over by Alloderm, which is a substitution for the muscle.
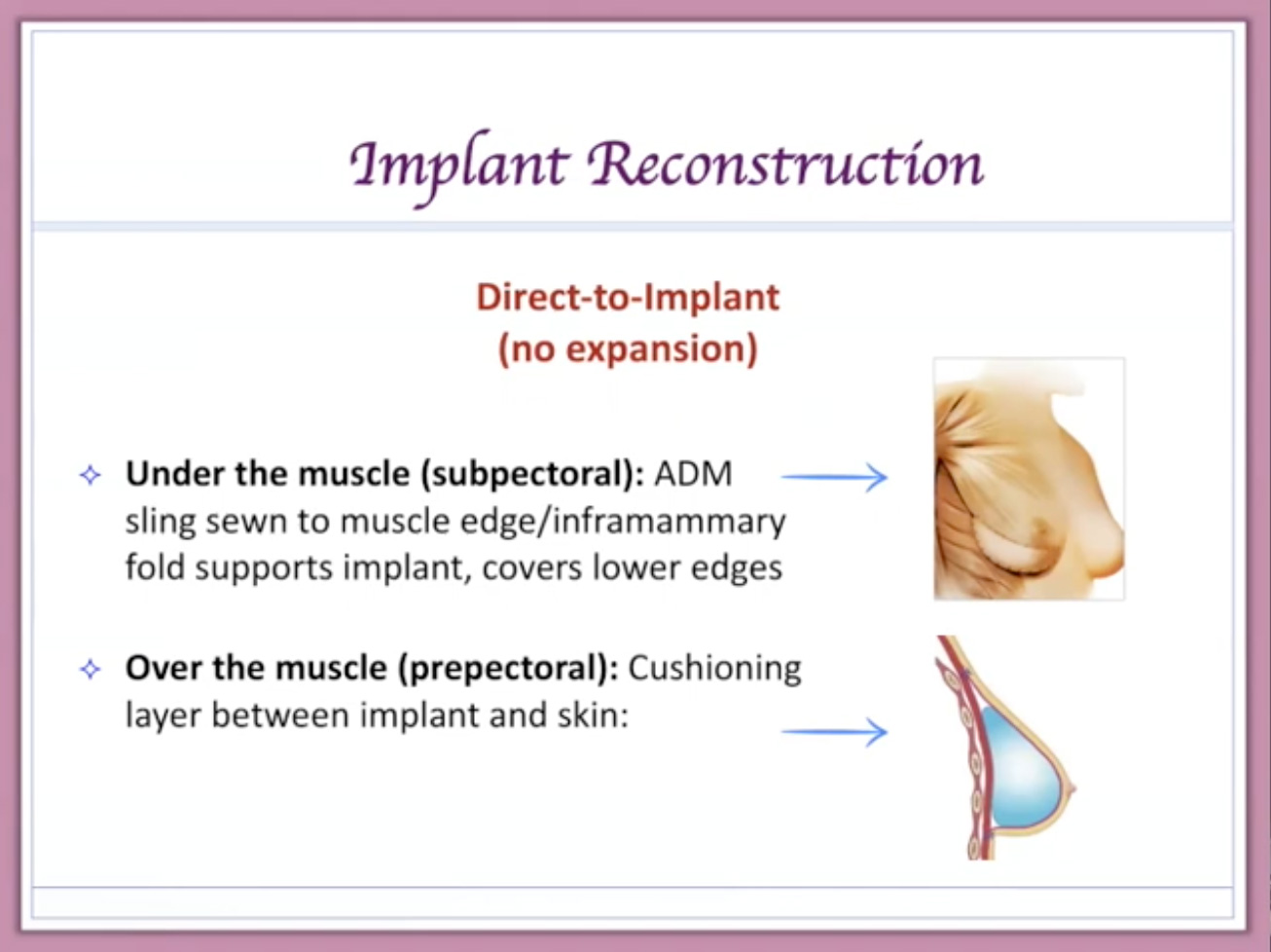
The advantages of direct to implant are that you don’t have to undergo expansion, there’s no second exchange surgery, and the patient wakes up with [00:13:12 a breast reconstruction.] Many of these operations are then improved or revised with fat grafting.
So, that covers the implant reconstructive procedures. Now, we’re going to turn into the other category, which is called autologous procedures. Now, autologous, again, refers to the fact that these are procedures using the patient’s own body tissue, and again, we also refer to these as flaps of living tissue. Now, the fact that it’s a flap of living tissue means that we get it from somewhere. That area is called the donor site, and at the donor site patients can expect another incision of course because we have taken that tissue from the patient’s own body. Now, these are procedures that require additional surgical skill and experience, and so not all plastic surgeons do all of these different procedures.
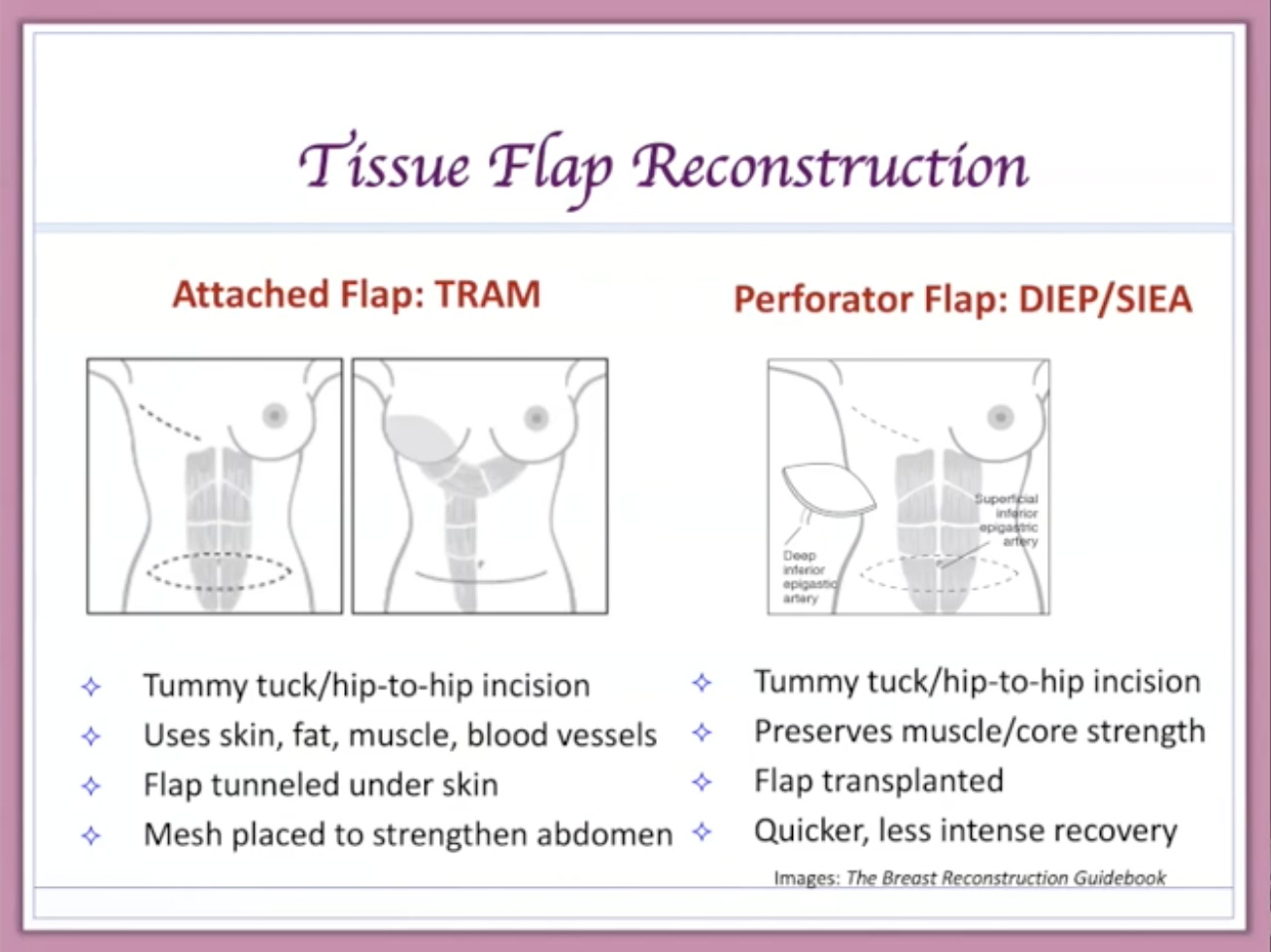
The procedure, again, involves using the patient’s own living body tissue and we take that tissue from an area on the body where it currently lives, and it lives by virtue of the fact that it has blood flowing through it. So, if we want to transplant living tissue to another part of the body, we have to do it in such a way that the blood continues to flow through it. Now, before we figured out how to take living skin and fat with its blood supply up into the chest, the only way to do that was to leave it attached to the underlying muscle, and those operations, which are still done in some places, are called pedicled flaps or attached flaps. Some that you may have heard of include the TRAM and the latissimus flaps, but those operations sacrifice a major muscle in the patient’s body. So, we’ve learned how to do the same operation with muscle preservation, and those operations are called perforator flaps, and those operations involve harvesting skin and fat and the blood vessel that supplies it but preserving the underlying muscle.
Again, the traditional or older procedures are called pedicled flaps and they involve muscle sacrifice. The newer procedures are called perforator flaps and they involve preservation of the underlying muscle.
This is a representation of those two options relative to the abdomen as a donor site. So, when we take the tissue from the abdomen as a pedicled flap, we’re taking the muscle along with the overlying skin and fat, and that operation is called a TRAM flap. Whereas with the perforator flap option that comes from the abdomen, we’re taking only skin and fat and the blood vessel that supplies it, and these operations are called perforator flaps and the one from the abdomen is called the DIEP. The DIEP is again just skin and fat and the blood vessel that supplies it, and this tissue is very delicately taken from the abdomen. The blood vessel is taken out of the muscle, preserving the function of the muscle such that you have skin and fat and blood vessel, which is then brought up to the chest, and those blood vessels are plugged into blood vessels in the chest to provide to the transferred tissue.
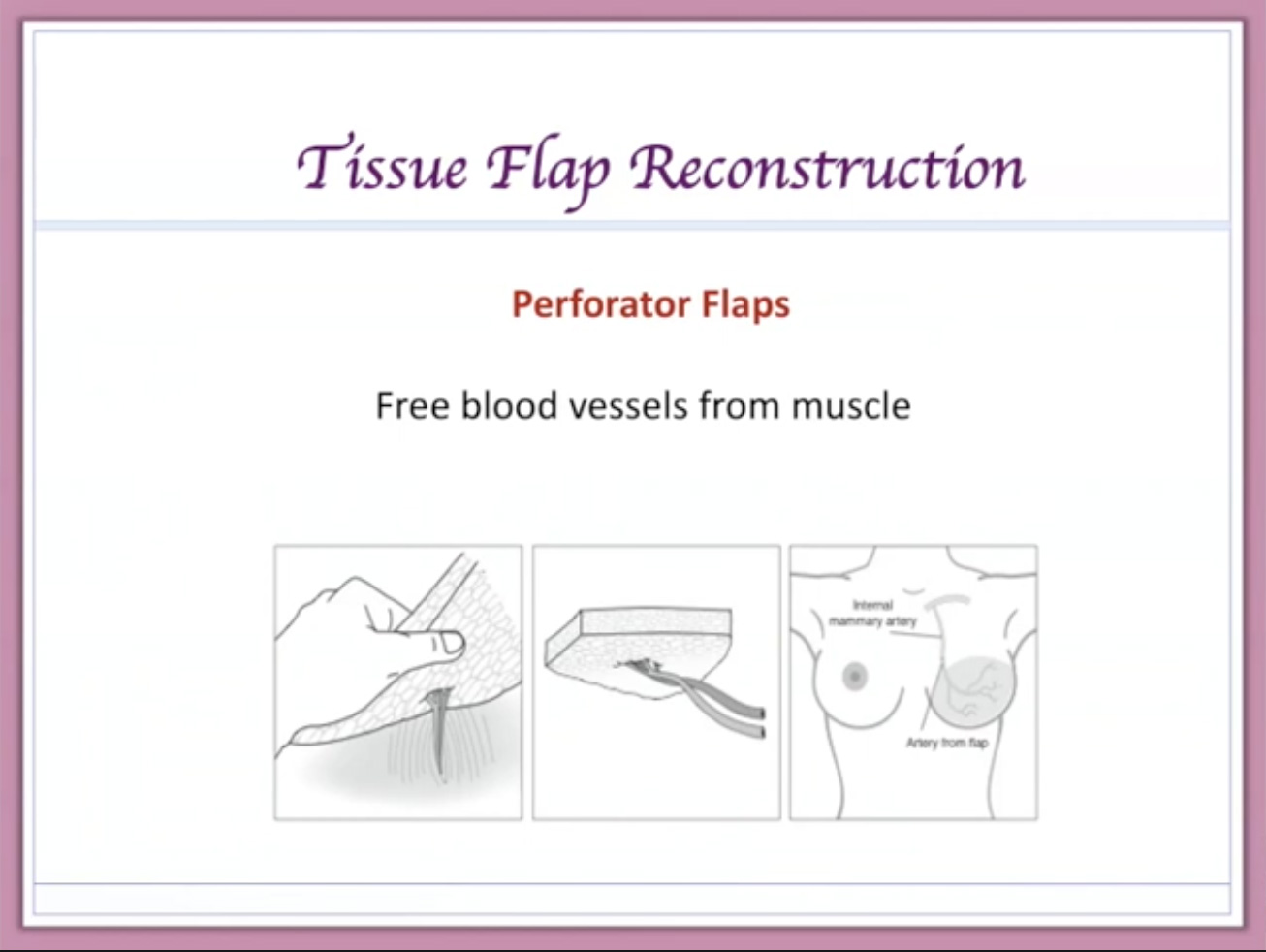
Now, the perforator flap that we’ve been talking about is called a DIEP and that one comes from the abdomen, but there are other options. So, wherever the patient has extra skin and fat a perforator flap can be used, and they have different names according to the area from which they are taken. But, the concept is always the same – skin and fat and the blood vessel that supplies it with the preservation of the underlying muscle, and that tissue is then transplanted to the chest and the blood vessels are plugged with a microscope.
Now, any type of breast reconstruction will almost always include a second followup procedure. We usually wait about three months for everything to settle down, and then we can go back and do a minor series of operations to improve the result by maybe changing the size – larger or smaller, maybe fixing issues with respect to symmetry, and we’re typically fixing minor defects with the breast reconstruction and with autologous tissue reconstruction at the donor area. Usually, we use that as an opportunity to do nipple reconstruction, which is another minor procedure, but many women now are opting to just have 3D tattooing, which provides the look of a nipple but without the operation, and the nipple tattoos have gotten so good that they really are very, very similar to nipple reconstruction. Some women get creative with nipple tattooing and even breast tattooing. So, this is always another option as well.
To ensure that you have the best chance of getting the outcome that you want as the patient, it’s very important to pick the appropriate plastic surgeon, and of course, the appropriate plastic surgeon is going to be different for different patients in different situations, but essentially you want someone who has a great deal of experience doing what they’re going to be doing for you. You should check on this person’s reputation and, ultimately, the relationship that you have with that surgeon is very, very important. Board certification is an absolute must, and I always recommend that patients seek at least a second opinion, and even a third opinion is advisable in some cases. The best thing you can do is learn about your options and learn the details of the different procedures that you’re considering, and so seeking more opinions if you have the time and if you can afford the time is always a good thing. You want to find a surgeon who can do what you want. In other words, asking a surgeon to do something that he or she is not comfortable with is never a good idea, and I always recommend to patients that they talk to other patients who have had this procedure and, particularly, other patients who have had this procedure by the surgeon that you’re considering going to.
So, when you’re trying to find a surgeon, what are you looking for? Well, you want someone obviously with a lot of experience, so you want to ask the surgeon very bluntly; How many of these procedures do you do on a monthly or annual basis? You want to know what is the surgeon’s success rate, and you want to know what you can expect – what is the best possible outcome, what is the worst possible outcome. You want to know how long surgery will be and what can you expect from recovery, and of course you want to know what are the potential risks of the surgery. If a complication does occur, what is the surgeon’s protocol for dealing with it? And, if you’re traveling for surgery, how does this surgeon handle a problem that happens after you’re back home?
What type of reconstruction you ultimately choose is a very, very big decision, it’s a very important part of your overall health and care with respect to how you’re dealing with either your prophylactic mastectomy or your mastectomy for cancer, and it’s a decision that sometimes comes at the end of the process wherein the patient goes in and is told that they need a mastectomy or they’re recommended to have a mastectomy, and then the mastectomy surgeon recommends a plastic surgeon and the plastic surgeon recommends a reconstruction, and the patient really will look back and say, “I never had the opportunity to think about this.” I would highly encourage you to put reconstruction at the top of your list in terms of choosing your team and in terms of choosing your treatment protocol because it is, ultimately, they’re one thing that you will be left with after all of this is done. [00:22:27 inaudible] have your breasts anymore; your risk will hopefully be eliminated. And so, when you look back, you’ll be looking at your breast reconstruction, and this is the thing that you will remember. So, it is a huge part of it and I would argue the part of the decision that should lead in the decision-making process. You have to think about things in terms of whether or not you’re willing to travel and what operation is ultimately best for you.
The decision, again, comes down to not only the reconstruction but of course the plastic surgeon, the breast surgeon, and all of you working together as a team – the patient, the breast surgeon and the plastic surgeon. So, I encourage you to talk to women who have been through this, talk to women who have been operated on by the surgeon that you are considering.
If you have any further questions, we have a breast panel scheduled during this conference and I will be participating in that along with two other very experienced plastic surgeons, and hopefully we’ll have the opportunity to answer any other questions that may remain for you.
I would also encourage you to become familiar with the FORCE website because it’s a tremendous resource for all things related to breast cancer, prophylactic mastectomy, BRCA gene mutation, and breast reconstruction. And again, I’ll mention the breast reconstruction guidebook written by Kathy Steligo, and thank you again Kathy for providing me with these outstanding slides. We really have provided here an overview, and again, if you want to get into more detail, I encourage you to attend our breast panel and we’ll try to continue to answer all questions related to breast reconstruction.
Thank you very much for your attention. I hope that this has been helpful.