This is restricted due to surgical images.
Mix & Match: A Staged Immediate Approach to Breast Reconstruction
Transcription of above presentation:
Hello, this is Dr. Joshua Levine. I’m a reconstructive microsurgeon in New York City and I do exclusively perforator flap breast reconstruction. In this presentation, I’ll be talking about the timing of breast reconstruction. In this particular presentation, I’ll be emphasizing the timing protocol that we call mix and match or staged immediate approach to breast reconstruction. Other terms that have been associated with this timing schedule include delayed immediate and staged breast reconstruction.
The timing of breast reconstruction can be variable. The mastectomy and the breast reconstruction are typically done at the same time. This is called immediate breast reconstruction.

Again, this means that a patient with breast cancer has a mastectomy or the removal of the breast and the reconstructive or plastic surgeon is there at the same time to do the reconstruction as soon as the mastectomy is completed during the same operation. This would be one hospital admission and one general anesthesia in order to do both the mastectomy and the reconstruction. Again, this is called immediate breast reconstruction. This approach is ideal in most circumstances but it’s not always available to everyone, and so whenever the reconstructive surgery is done at a later time, after the mastectomy has already been done, whether it’s within the next few days or in the next years, we call that delayed reconstruction.
More recently, we have found the need to offer a hybrid which we call delayed immediate or staged reconstruction. This is when we actually plan to provide the mastectomy for the patient on one day, without reconstruction, knowing that we’re going to bring the patient back a week or two weeks up to even several weeks later to do the reconstruction. We call that delayed immediate or staged reconstruction.
Just do digress a moment, I’d like to say a couple of things about nipple-sparing mastectomy.
Many women who are diagnosed with breast cancer are very young or women may be having mastectomies who don’t have cancer at all. In this case, we call it prophylactic mastectomy, and these patients are patients who have identified a very high risk for developing breast cancer in the future or they may have been found to have the BRCA or other gene mutations which predispose them to a very high risk of breast reconstruction. Many times, women today are seeking to have nipple-sparing mastectomy in order to improve the cosmetic outcome of the breast reconstruction. Nipple-sparing mastectomy means that the mastectomy is performed, the entire breast is removed, but the nipple and the areola are left. The reason someone would want this is because it does provide, in ideal circumstances, the best cosmetic outcome that we can achieve with reconstructive surgery.
Nipple-sparing is not without risks and potential complications and one of them is similar to what could happen to any skin after a mastectomy, which is skin necrosis. When a mastectomy is done, a large portion of the blood supply leading to the skin is removed and this leaves the skin and particularly the nipple at risk of having poor blood flow, and this can lead to skin necrosis of the mastectomy skin or nipple necrosis. Another potential problem with nipple-sparing mastectomy is nipple malposition, particularly in cases where one has a large mastectomy volume and a smaller amount of volume to replace for the reconstruction.
In order to deal with some of these problems, a colleague in North Carolina, Michael Zenn, developed what he called the Zenn delay, and the idea of this was to minimize problems associated with skin and nipple necrosis, and this was related to implant reconstruction.
He found that if the mastectomy was done on one day and the skin and nipple were significantly traumatized or the blood supply had been damaged to the remaining skin and nipple that the patient would benefit from not having an immediate reconstruction, in other words, not going ahead with a planned reconstruction in order to give the skin and nipple time to recover, and in doing so he found that the number of problems and complications associated with poor perfusion to the nipple and to the skin went way down almost to zero.
We have begun to apply the same concept to autologous reconstruction, and I will be describing that in a few minutes. First, let’s talk about how it works. The patient who is a candidate for this would plan to have the mastectomy done on one day with one surgeon and then, after the patient recovers from that surgery, which is generally within 24 hours, the patient will be discharged from the hospital and plan to have the breast reconstruction approximately one week later, but it could be much more than that depending on the circumstance.
There are several advantages to this approach.
First of all, the breast surgeon and the plastic surgeon operate independent of one another. Also, the patient can choose any breast surgeon that she likes in any location or circumstance that she finds herself and choose a reconstructive surgeon that doesn’t necessarily have the ability to operate with that surgeon at the time of the mastectomy. Therefore, it opens up the options for which surgeons the patient can choose. The patient may want to choose different surgeons from different hospitals or different teams or even different states based on preference, based on a prior relationship that the patient may have with her treating physicians or based on geographical concerns. In other words, the breast surgeon or plastic surgeon that she would like to use may not live within a certain area, making it impossible for her breast surgeon and her plastic surgeon to work together simultaneously. So, this gives the patient a great deal more choice and control over the surgical teams that she uses and the outcome that she expects.
This is a young patient with known BRCA gene mutation.
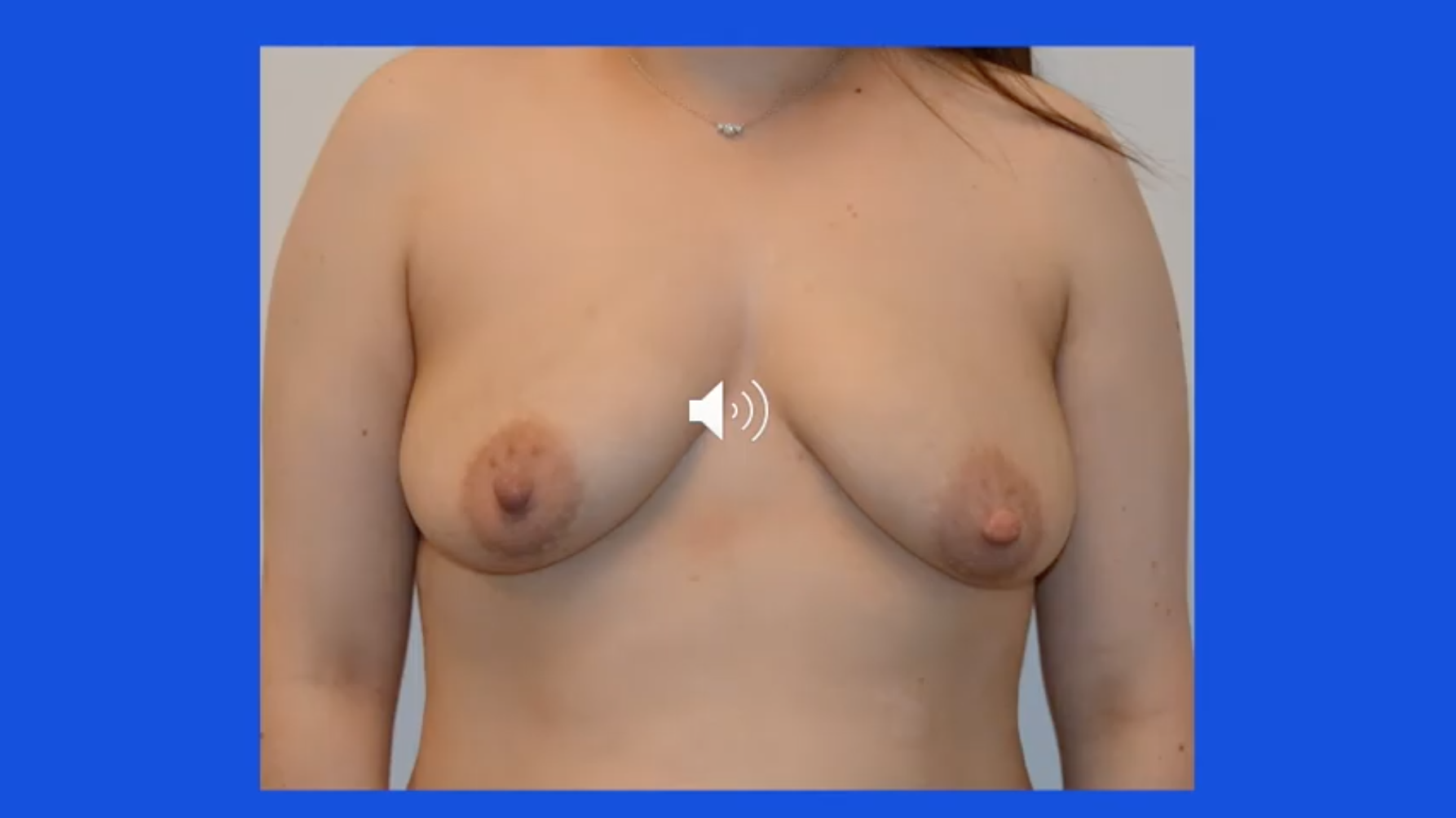
She came in seeking autologous breast reconstruction but could not find the appropriate plastic surgeon at her institution in her hometown to perform this operation. She went ahead and had the bilateral mastectomies performed and scheduled for autologous reconstruction for a week later. The patient underwent bilateral nipple-sparing mastectomy through an inframammary incision, which is underneath the breast. She recovered from the procedure, was discharged from the hospital, and she was scheduled to have her autologous breast reconstruction one week later. Her bilateral DIEP breast reconstruction was done at a different hospital one week later.

This is another patient who has the BRCA gene mutation and wanted to have bilateral prophylactic nipple-sparing mastectomy in her hometown with a surgeon whom she trusted.

High-level sophisticated perforator flap breast reconstruction was not offered at that time at her hospital, so she elected to have delayed immediate or staged breast reconstruction. She underwent bilateral nipple-sparing mastectomies through an inframammary incision on one day, was discharged from the hospital the following day, and had her bilateral DIEP flap breast reconstruction performed at a different hospital one week later.
Immediate breast reconstruction is the standard of care. In other words, ideally all patients would have access to the mastectomy surgeon of her choice and the reconstructive surgeon of her choice, and those two individuals could work together at the same time. However, this is not always the case, and the question comes up, “Can a patient mix and match?”
In other words, can she choose the breast surgeon that she’s most comfortable with and the plastic surgeon that she’s most comfortable with? The answer is yes, the patient can find the appropriate surgical team. They may not be able to work together simultaneously, and in this circumstance, we call this the delayed or staged immediate. The patient can choose the breast surgeon that she feels most comfortable with and the reconstructive surgeon that she feels most comfortable with, and these procedures can be done in a staged fashion such that the mastectomy is done on one day and the reconstruction is done at a later date. This offers the advantage of the patient having the surgeons of her choice, and it also has the advantage of having the highest probability of nipple survival and skin health at the time of the reconstruction.
This concludes the presentation on staged immediate. I hope that this has been helpful.